Connect With Us
Blog
Items filtered by date: Thursday, 08 May 2025
Causes of Foot Arch Pain

Foot arch pain is often due to prolonged pressure on the feet. Muscles and tendons that support the arches can become fatigued, leading to discomfort, especially for those with an active lifestyle. The most frequent cause of foot arch pain is plantar fasciitis, marked by damage to the thick band of tissue under the foot. It typically develops from altered foot biomechanics, bone spurs, and muscle tightness. Foot cramps, which affect 25 percent of individuals who are 60 and older, contribute to sudden, intense muscle spasms and arch pain. Tarsal tunnel syndrome, though less common, results from pressure on the tibial nerve, causing inner arch pain, pins and needles, and numbness. Plantar fibromatosis involves small nodules in the plantar fascia, causing a firm lump in the arch and pain with pressure. Posterior tibial tendonitis, often the result of overuse during high-impact activities, leads to pain on the bottom of the foot. Stress fractures, commonly caused by repetitive overloading during high-impact activities, result in sharp arch pain with localized bruising and swelling. Additionally, flat feet, where arches collapse, are linked to foot arch pain as well as knee and back pain. Custom orthotics can alleviate discomfort from foot arch pain. For a solution to foot arch pain, it is suggested that you schedule an appointment with a podiatrist.
If you have any concerns about your feet, contact Tanisha Richmond, DPM from Richmond Foot & Ankle, LLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Dayton, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics in Podiatry
Podiatry is a branch of medicine that deals with the study, diagnosis, and treatment of foot and ankle conditions. There are various subdivisions in podiatry; biomechanics is one of them. Biomechanics is the way in which the bones, muscles, and joints of the feet and lower limb interact with each other.
Our feet play crucial roles in the way we move, and it is rare to have feet that are completely symmetrical. Common biomechanical issues include high or low arches or uneven leg heights. Excessive pronation often leads to fallen arches, or flat feet, and is a common cause of running injuries. People whose feet are over-pronated tend to have flexible and unstable feet. Pain is usually experienced during walking and running.
At times, people may be able to adapt to these abnormalities without any difficulties, but in other cases, these issues can cause a great deal of pain. This pain occurs because the joints, muscles, ligaments, and tendons are put under an excess amount of stress during movement. Common symptoms of biomechanical problems stemming from the feet include hip pain, knee pain, leg cramps, ankle pain, lower back pain, weak ankles, tripping, heel pain, Achilles pain, and shin splints.
Many biomechanical issues can be treated with orthotics. Orthotics are shoe insoles that are used to help control the way the foot operates. They can provide relief from foot pain, heel pain, and knee pain. Depending on your specific case, you may need to purchase over-the-counter orthotics or custom orthotics to fit your feet. Your podiatrist will be able to prescribe the perfect orthotic for your feet to help you walk around with ease.
Gait is defined as the way we move our bodies from one point to another. This is usually done by either walking or running. Gait analysis is a method used to assess the way we walk or run to highlight biomechanical abnormalities. Gait analyses are a great way to take a detailed look at how you walk and how your foot moves while you walk. An examination of the feet will help your podiatrist understand why you are suffering pain in other parts of your body.
It's Time for Beautiful Feet
What Is a Diabetic Foot Ulcer?
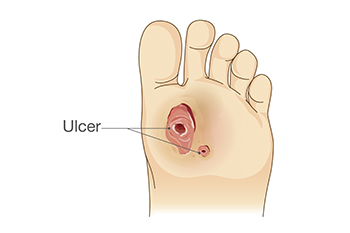
A diabetic foot ulcer, a grave complication for individuals with diabetes, is a chronic open sore that develops on the feet, typically on the bottom or sides. It arises from a combination of factors intricately linked to the effects of diabetes on the body. Diabetes can lead to neuropathy, causing reduced sensation in the feet and making it challenging to detect injuries or pressure points. Additionally, compromised blood circulation hampers the healing process, increasing the risk of infections and the formation of ulcers. Contributing further, the elevated blood sugar levels associated with diabetes impair the immune system, increasing the risk of infections. Foot ulcers, if left untreated, can escalate into serious complications and be quite painful. Recognizing the effects of diabetic foot ulcers underscores the importance of meticulous foot care in diabetes management. If you have diabetes and have developed a foot ulcer, it is suggested that you are under the care of a podiatrist who can effectively treat this type of wound, and help you to manage this condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Tanisha Richmond, DPM from Richmond Foot & Ankle, LLC. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Dayton, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Causes of Stress Fractures

Engaging regularly in high-impact activities, like basketball, running, or professional dancing, may expose you to the discomfort of a foot stress fracture. This overuse injury involves hairline cracks in weight-bearing bones of the foot. If left untreated, a stress fracture in the foot can escalate into a more serious concern. However, stress fractures are not always easy to diagnose. Pain upon weight-bearing activities that often subsides after rest is a primary indicator of stress fractures. Tenderness in the affected area, occasional bruising, and swelling around the ankle are other signs to be noted. Various factors contribute to the development of stress fractures in the foot. Overuse and repetitive stress, stemming from prolonged engagement in activities without adequate rest, can subject the foot bones to cumulative stress. Wearing inadequate footwear, whether ill-fitting or worn-out, further elevates the risk by providing insufficient support and shock absorption. Additionally, suddenly increasing the intensity or duration of physical activity can overwhelm the bones, especially without sufficient time to adapt. Nutritional deficiencies, particularly in calcium and vitamin D, can weaken bones and make them more susceptible to hairline fractures. If you believe you may have incurred a foot stress fracture, it is suggested that you make an appointment with a podiatrist for a thorough exam and suitable imaging tests and treatment options.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Tanisha Richmond, DPM from Richmond Foot & Ankle, LLC. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Dayton, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Heel Pain Can Be Treated!
The Precise Nature of Laser Treatment for Fungal Nails

Laser treatment for fungal nails, a therapeutic modality gaining prominence, involves utilizing concentrated beams of light to target and eradicate fungal infections within the nail bed. This non-invasive procedure harnesses the power of specific wavelengths to penetrate the nail and reach the underlying fungal colonies, without causing harm to surrounding tissues. The laser energy is absorbed by the pigments in the fungal cells, generating heat that neutralizes the infection. Unlike traditional treatments, laser therapy poses minimal risk of side effects and does not necessitate medications. The exact mechanism of laser treatment for fungal nails underscores its precision, selectively targeting the fungal pathogens while preserving the integrity of the nail and surrounding structures. If you have toenail fungus, it is strongly suggested that you speak with a podiatrist who can determine if laser treatment is the correct treatment option for you.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with Tanisha Richmond, DPM from Richmond Foot & Ankle, LLC. Our doctor will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
- Nail thickening
- Brittleness of the nail
- Discoloration of the nail
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact our office located in Dayton, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Laser Treatment for Fungal Nails
A new treatment for fungal nails, or onychomycosis, which has grown in popularity in recent years, is laser treatment. Laser treatment involves the use of a laser that kills fungus in the toenail with heat. Laser therapy causes no side effects and does not affect nearby healthy tissue.
Toenail fungus afflicts almost 10 percent of the U.S. population and is more common among the elderly. The most common symptom of toenail fungus is the discoloration and thickening of the nail. The nail can also become brittle and a foul smell may be produced. In rare cases, pain might be present. While it is not a serious condition, it can lead to a perception of disgust amongst those it affects. There are several different fungi that cause fungal infections. These include dermatophyte, yeast, and mold. The most common of these is dermatophyte.
Diagnosis for fungal nails involves a podiatrist utilizing microscopy and fungal cultures. This will allow the doctor to determine whether it is a fungus or another condition, such as lichen planus, psoriasis, nail damage, and onychogryphosis.
Fungus in the nails can be hard to get rid of with over-the-counter drugs. This is due to the nail being hard and protective, with fungus able to slip between the nail bed and plate. Furthermore the slow growth of the nail increases the difficulty of fungus going away. Laser treatment seeks to get around this by directly penetrating through the nail and killing the fungus. The laser is used on each infected nail for a couple of minutes. Patients then typically return several weeks or months later for another laser treatment. During this time the podiatrist will routinely observe the foot and infection. It is also recommended to wear clean socks and shoes and allow the feet to dry and breathe to prevent toenail fungus.
Laser treatment is still a relatively new treatment and not all podiatrists have laser machines. Ask your podiatrist if they do laser treatment for toenail fungus and if it is right for you.
Blog Archives
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018